What are the differences between a respirator and face coverings?
Normally, in industrial hygiene, we think about wearing respiratory protective equipment (RPE) to protect people from harmful contaminants such as asbestos, mould, and benzene. However, we now have to consider that people can be the source of harmful contaminants by breathing out the COVID-19 virus. Until recently, only surgical masks were used to protect the people not wearing a mask, such as when a doctor wears a mask during surgery to protect the patient.
So, in general, we consider a respirator to protect the wearer, and a face covering to protect other people from the wearer.
Respirators
A respirator is a device designed to protect the wearer and has undergone rigorous testing to determine its effectiveness. Although respirators are designed to protect the wearer, there has not been consideration for it to protect others from aerosols being expelled by the wearer.
- Air purifying respirators have filtration and work under suction to aid face seal.
- Air supplying respirators and powered air-purifying respirators (PAPRs) have a positive pressure so the face seal becomes less important.
For RPE, the device must be fit tested to ensure it fits properly and is worn correctly to ensure it will work as designed to protect you from contaminants. See our blog on fit testing for more information on ensuring your RPE is functioning properly: https://www.cihc.info/respirator-fit-testing-how-do-i-know-my-respirator-actually-works/
Face Coverings
A face covering is a device placed on the face to act as a form of source control to reduce the amount of moist particles expelled from the wearer’s nose and mouth. They may not really count as RPE.
How Effective Are Cloth Face Coverings at Reducing the Spread of COVID-19?
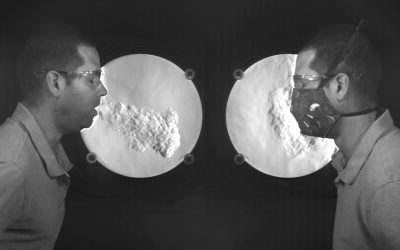
A University of Edinburgh study showed that face coverings deflect the user’s breath up or down, and sometimes backwards. This means the obvious benefit of face coverings is that they prevent forward projection of exhaled breath, but one should use caution when standing beside or behind the user.
At the same time, a German study (the Aeromask Project) indicated that masking effectively slowed down the exhaled breath and the thermal effects of body heat made particles stay close to the body. In calm air, the particles floated toward the ceiling and spread slowly through the room in a more diluted manner. Ventilation becomes really important as it will determine whether there are pockets of contaminated air that lingers, and potentially exposing people.
How effective are cloth face coverings at reducing the spread of COVID-19?
So, while the exhaled breath may leak out the sides and behind the spreader, it should at some level stay close to the body then lift. Even when masks are worn it’s best to adhere to physical distancing measures.
How Effective are Surgical Masks at Reducing the Spread of COVID-19?
Surgical masks are designed to protect the patient from the doctor, not the doctor from the patient. The US FDA recommends that manufacturers demonstrate surgical mask performance in four areas:
- fluid resistance,
- filter efficiency,
- differential pressure, and
Two types of filter efficiency tests are recommended:
- particulate filtration efficiency (PFE) and
- bacterial filtration efficiency.
The FDA requires no minimum level of filter performance. The CDC publishes guidelines on the use of surgical masks in health care settings.
The International Society for Respiratory protection says that surgical masks protect against bodily fluids to the nose and mouth and recommends placing them on potentially infectious patients to limit spread of infection from one patient to another.
Since surgical masks are actually designed for the purpose of acting as source control, they will likely be more effective than cloth face coverings. They will also have the same leakage issues as cloth face coverings, but are more prone to leakage behind the user.
How Effective are Respirators at Reducing the Spread of COVID-19?
Often, respirators have a one-way valve called an “exhalation valve” which when you inhale, pathogens cannot get in, but when you exhale your breath is not filtered.
Masks with exhalation valves; in particular, N95 or elastomeric respirators (with P-100 cartridges) will provide the best protection against the ingression of virus particles and droplets into the user’s airway. However, the exhalation valve becomes problematic for source control as the exhaled air is not filtered.

How effective are respirators at reducing the spread of COVID-19?
One possible solution is to put a face covering over top of the exhalation valve, thus capturing the droplets, which allows maximum protection for the user and it acts as source control.
N95s without exhalation valves can also be purchased, which would act optimally as source control and as RPE.
How Effective are Face Shields in Reducing the Spread of COVID-19?
In a study reported by the Guardian, Riken in Japan used a supercomputer simulation and found that almost 100% of airborne droplets less than 5 micrometers in size escaped through plastic visors and half of larger droplets measuring 50 micrometers found their way into the air. This makes it essentially the least effective of measures people are currently using as face coverings.
One of the researchers, Makoto Tsubokura suggests that those who are not advised to wear masks, such as those with underlying respiratory conditions and small children could wear face shields instead, if that is their only option, but only outdoor or in indoor settings which are properly ventilated.
Conclusion
N95s without an exhalation valve would be the best of both worlds, acting as RPE and source control; however, they may be in limited supply at different period in the pandemic and there is an environmental issue with continuously disposing of them after usage.
Surgical masks are likely the next best option for source control as they are actually designed for that purpose, but they also become an environmental issue with continuously disposing of them after usage.
Reusable fabric face coverings are more accessible to the general public and are reusable and depending on the fabric type (which we will get into in a subsequent blog), can be very effective. It does need to be noted that their limitation is that there is leakage sideways and backwards, so physical distancing is still vital, as is the case with surgical masks.
Respirators have limitations as a form of source control if they have an exhalation valve. The exhalation valve should be covered when around other individuals without respirators.
If you have been advised to not wear a face covering, a face shield is a good option but should only be considered sufficient outdoors and in well ventilated areas.
Resources
The Aeromask Project – How effective are non-medical masks? – 2020 https://bit.ly/3lMTjix
ACS Nano – Aerosol Filtration Efficiency of Common Fabrics Used in Respiratory Cloth Masks
2020 https://pubs.acs.org/doi/pdf/10.1021/acsnano.0c03252
Jeremy Howard et. Al – Face Masks Against COVID-19: An Evidence Review – 2020 https://bit.ly/2JGWOdq
Oberg & Brosseau – Face Masks Against COVID-19: An Evidence Review – 2020 https://bit.ly/33RaGZA
The International Society for Respiratory protection – Filtration Performance of FDA-Cleared Surgical Masks https://bit.ly/3lTJcZA
ScienceDaily – New airflow videos show why masks with exhalation valves do not slow the spread of COVID-19 – 2020 https://bit.ly/2VSjp9i
The Guardian – Face shield ineffective at trapping Aerosols – 2020 https://bit.ly/3gfRUQv
ISRP 2020: The Role of Respiratory Protection in Response to Coronavirus: European Response to SARS-Cov2 (COVID-19) Outbreak https://youtu.be/lyJGgZYCTAI
What is a mask valve, and why are cities banning them? – Fast Company – 2020
https://images.fastcompany.net/image/upload/w_1153,ar_16:9,c_fill,g_auto,f_auto,q_auto,fl_lossy/wp-cms/uploads/2020/04/p-1-90496717-what-is-a-mask-valve-and-why-are-cities-banning-them.jpg
The Do’s and Don’ts of Face Coverings – GBMC – 2020 https://www.gbmc.org/the-dos-and-donts-of-face-coverings

